A Tale of Two Glutens: Mensch or Monster?
There once was a protein named Glutey. Around the world, chefs and bakers invoked Glutey's magic by kneading their dough. The more the dough was kneaded, the stronger Glutey became. Glutey was renowned for his remarkable ability to manipulate the texture of products derived from wheat, rye, barley and spelt, among others. Oh, the chewy goodness!
Grains without gluten
- Corn
- Rice
- Buckwheat
- Oats
- Teff
- Quinoa
Gluten--literally "glue" in Latin--provides an elastic consistency to dough. The next time you take a bite out of bread, evaluate the chewiness. The chewier the bread, the more glutinous the bread. Compare this to flakey pastries which have a much lower gluten content.
The agricultural revolution dramatically increased the amount of gluten in the diets of human beings, especially the wheat-heavy societies in Europe and the Middle East. Unfortunately, Glutey rubbed some people the wrong way, whether they knew it or not. Some experienced immediate aversions to gluten-containing products, whereas others suffered more subtle, chronic effects.
It wasn't until the second half of the 20th century that Glutey would be indicted as the little-known monster lurking in that challah roll, that tagliatelle, that brewski, that mock duck. A proteinaceous pest eager to wrangle your insides and leave you bloated and gassy, or worse.
So, manufacturers created a market of gluten-free products catering to Celiacs. But 1% of the American population simply wasn't enough. So, they planted a grain in the hungry minds of Americans: there is a toxin looming in your carbohydrates, beware! What originated as a niche product for a sliver of the population has exploded into a massive industry. The global market for gluten-free goods exceeded USD 4 billion in 2015.
So, is gluten really the monster it's made out to be? For some, yes, even deadly. But the truth is, the overwhelming majority of Americans can consume gluten without incident: no anaphylactic reaction, no gastrointestinal explosion, no symptoms whatsoever. That is, unless you have one of the three main gluten-related disorders.
3 Gluten-Related Disorders
MORE SEVERE
Wheat allergy: Allergic, occurring over minutes to hours
Celiac disease: Autoimmune, occurring over weeks to years
Gluten sensitivity: Immune-mediated, occurring over hours to days
LESS SEVERE
Wheat allergy
In someone who has wheat allergy, the immune system perceives gluten to be a malicious invader, which can lead to a potentially life-threatening cascade of reactions: narrowing of the airway, decrease in blood pressure and even death. Better have that epi pen! #Anaphylaxis.
Wheat allergy can also produce gastrointestinal symptoms similar to celiac disease; however, what distinguishes the two is the time frame: wheat allergy occurs almost immediately, whereas celiac disease produces symptoms hours to months after ingestion, if it produces symptoms at all.
Wheat allergy can be tested by skin prick, blood test for IgE antibodies or a gluten challenge.
Celiac disease
The textbook presentation is pale, loose, greasy diarrhea and many of the symptoms overlap with Irritable Bowel Syndrome. Some Celiacs experience extra-intestinal symptoms, while still others notice no symptoms at all.
Everyone thinks she's a celiac. Not true, bae. Only about 1% of the Western world suffers from this gluten-related disorder.
Celiac disease is a type of autoimmune disease--an abnormal response of the body's immune system against itself--and occurs in genetically susceptible individuals.
An enemy is perceived from within.
In Celiac disease, the attack is launched against the lining of the small intestine. How? The immune system creates autoantibodies against the lining of the small bowel. The two most commonly implicated autoantibodies are anti-tTG [tissue transglutaminase] and anti-EMA [endomysial]. A positive blood test for either of these antibodies supports a diagnosis of Celiac disease and warrants further investigation.
Criteria supporting Celiac Disease
- Symptoms characteristic of Celiac Disease
- Presence of IgA autoantibodies
- Genetic predisposition HLA-DQ2 or HLA-DQ8
- Small bowel biopsy showing characteristic damage
- Improvement on a gluten-free diet
Can anyone form autoantibodies against the lining of her small intestine? In theory, yes. But, formation of these autoantibodies is much more likely if you inherited certain genes from your parents. Named HLA-DQ2 & HLA-DQ8, these alleles are found in nearly everyone who has Celiac disease. A blood test can check if you inherited either of these from your parents. Absence of these alleles essentially rules out Celiac disease; however, their presence alone does not confirm the disease.
Ultimately, confirmation occurs with upper endoscopy. I hope there's no celiac disease in heaven @Joan_Rivers!
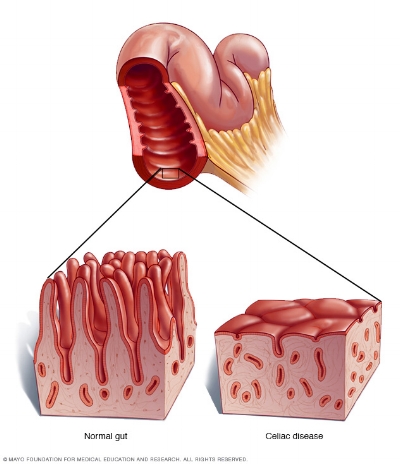
The next time someone cites her celiac disease, demand the pathology report from her endoscopy. This is the gold standard for diagnosis. Remember those autoantibodies? True celiac disease is characterized by autoantibody-induced damage to the villi, or finger like projections of the small intestine. The villi increase surface area and are responsible for absorption of nutrients. For this reason, a person with undiagnosed celiac disease may exhibit complications of malabsorption such as diarrhea, iron deficiency and osteoporosis.
Of note, because Celiac disease is autoimmune, Celiacs have a higher risk of other autoimmune disorders like type 1 diabetes, Multiple Sclerosis, thyroiditis, rheumatoid arthritis, Sjögren's Syndrome, etc.
WHY A CELIAC MAY TEST NEGATIVE FOR CELIAC DISEASE
If a Celiac removes gluten from her diet, the immune system will stop generating autoantibodies and the small bowel will regenerate itself! Of course, this means that blood tests for autoantibodies and the endoscopy would yield negative results. That's why anyone concerned she has a gluten allergy should be maintained on a gluten-rich diet leading up to tests for Celiac disease.
Gluten sensitivity
In the hubbub of celiac disease, whispers of gluten sensitivity took root. Perhaps you don't have celiac disease, but certainly you have gluten sensitivity. Banish this toxic protein from your diet!
The typical presentation is a combination of Irritable Bowel Syndrome like symptoms (e.g. abdominal pain, diarrhea, constipation, bloating) and systemic symptoms (e.g. fatigue, headache, joint and muscle pain). This constellation of symptoms disappears after switching to a gluten-free diet.
Gluten sensitivity can only be diagnosed after wheat allergy and celiac disease have been excluded. However, there is no definitive biomarker to confirm this gluten-related disorder, thus fanning the flames of the gluten hysteria.
Although gluten sensitivity is immune-mediated, it is not autoimmune like celiac disease. Rather than produce antibodies directed against the small bowel, the immune system produces antibodies against wheat itself. Unlike the IgE antibodies of wheat allergy and IgA antibodies of celiac disease, these are less specific IgG antibodies. The problem? Some people will test positive for these antibodies even if they have no symptoms of gluten sensitivity. While testing for the antibodies is non-specific, it's definitely a start for anyone concerned about sensitivity to gluten.
Want to test for antibodies against gluten and other foods that you regularly consume?
Sometimes, it's not so obvious that your immune system is producing antibodies against foods in your diet. Food sensitivity testing can identify dietary culprits that may be producing various maladies, such as: migraines, joint pain, nausea, diarrhea, etc. Examine the sample report below. Removing these foods from your diet should reduce any symptoms you have and improve your quality of life.
Are you ready to find out if you have any food sensitivities? Schedule an appointment today.
Works Cited
Catassi C, Bai JC, Bonaz B, Bouma G, Calabrò A, Carroccio A, Castillejo G, Ciacci C, Cristofori F, Dolinsek J, Francavilla R, Elli L, Green P, Holtmeier W, Koehler P, Koletzko S, Meinhold C, Sanders D, Schumann M, Schuppan D, Ullrich R, Vécsei A, Volta U, Zevallos V, Sapone A, Fasano A (Sep 2013). "Non-Celiac Gluten sensitivity: the new frontier of gluten related disorders". Nutrients. 5 (10): 3839–53. doi:10.3390/nu5103839
Sapone A, Bai JC, Ciacci C, Dolinsek J, Green PH, Hadjivassiliou M, Kaukinen K, Rostami K, Sanders DS, Schumann M, Ullrich R, Villalta D, Volta U, Catassi C, Fasano A (2012). "Spectrum of gluten-related disorders: consensus on new nomenclature and classification". BMC Medicine (Review) 10: 13. doi:
Tovoli F, Masi C, Guidetti E, Negrini G, Paterini P, Bolondi L (Mar 16, 2015). "Clinical and diagnostic aspects of gluten related disorders". World J Clin Cases (Review). 3 (3): 275–84.